The literature confirms that women with euploid losses have a higher risk
of recurrent loss if not treated.
We previously reported a high success rate in women with a history 5 or
more miscarriages-80% (a group with high probability of euploid losses).
We now report on a larger series of women with a history of at least one
euploid loss, a group of patients that most likely have immune related
implantation issues.
First results of our retrospective study based on 90 cases under our care showed a
live birth rate of 77.8% as seen in Figure 1 (p=.0001, a very low p value shows a very high statistical
significance).
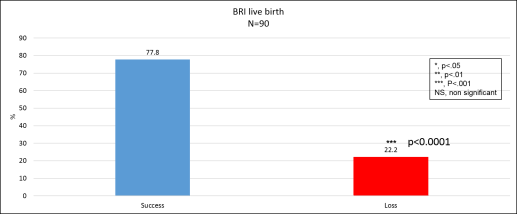
Figure 1: Live birth rate at Braverman Reproductive Immunology in women
with at least 1 euploid loss and after adequate immune therapies.(This
is not a guarantee of future performance).
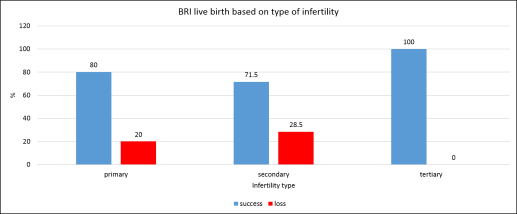
There was
no significant difference between the different types of infertility as shown in Figure 2.
- Primary has no history of a successful birth prior to the miscarriages
- Secondary has a history of a full term birth followed by miscarriages
- Tertiary has a history of miscarriages prior to and after a full term birth
Figure 2: Live birth rate at Braverman Reproductive Immunology in women
with at least 1 euploid loss and after adequate immune therapies based
on the type of infertility.
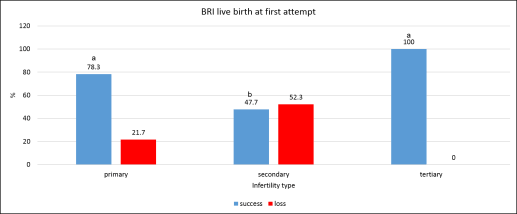
Now, if we consider only
the first attempt to conceive,
71%
of our patients will get a successful pregnancy as seen in Figure 3 (p=.0001, a very low p value shows a very high statistical
significance).
Figure 3: Live birth rate at Braverman Reproductive Immunology at first
attempt in women with at least 1 euploid loss and after adequate immune
therapies.
We defined euploid losses as pregnancies losses with:
- aCGH on the product of conception (POC) showing euploid (normal) karyotype
- Normal PGD (Preimplantation genetic diagnosis) tested embryo with a fetal
heartbeat (FHB) detected prior to the loss
- Clinical pregnancy (>6 weeks) with a FHB detection prior to the loss
ALL patients who had immune work done with us were included in the study with the
ONLY exclusion being uterine anomalies. Patients received our tailored immune
therapy based on their results prior to conception (natural conception
or IVF cycle), and the treatment was maintained at least through the first
trimester.
The pregnancy outcome was recorded retrospectively with a successful pregnancy
being defined as a live birth or an ongoing pregnancy of more than 20 weeks.
As discussed in our previous blog on women with at least 5 losses (add
the link), women with euploid losses are at higher risk for further losses.
Patients with a history of aneuploidy miscarriages (abnormal genetics)
, do not appear to be at increased risk for recurrent losses.
1- Review of the current literature on recurrent pregnancy loss statistics.
a. Ogasawara and collaborators1
They showed that the likelihood of a loss being normal (euploid) was higher
in recurrent miscarriage patients (48.7%) compared to the control population
of those having a miscarriage for the first time (23.7%).
Interestingly, the frequency of an
aneuploid (abnormal) loss significantly
decreased
with the number of previous miscarriages, while that of a
normal loss (euploid) significantly
increased. Showing a likely cause and not just a random one.
b. Morikawa and collaborators2
They showed that RPL patients are more prone to have another euploid loss
confirming these results.
In this study, euploid losses were shown to be significantly higher in
RPL patients (66.7%) vs. controls (45.7%) while aneuploid losses remain
the same between the two groups. Again this shows that it is the euploid
losses that most likely need treatment.
c. Carp and collaborators3
They focused on genetic testing on products of conception in patients with
3 or more miscarriages. They found that the incidence of aneuploid losses
among these miscarriages was 29% while 71% of losses were euploid. They
also estimated that after an aneuploid loss, 68% will have a live birth
while after euploid losses only 41% will have a live birth.
Altogether these data clearly show
that patients with high number of miscarriages are most likely to lose
euploid pregnancies and these types of losses tend to reoccur without
treatment.
1. Comparing our success at BRI against the published literature
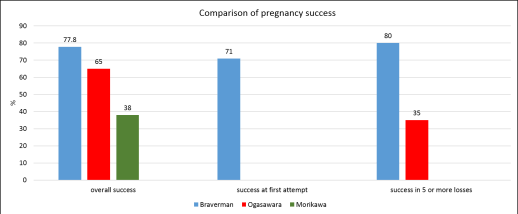
Figure 5: Pregnancy success rate at Braverman Reproductive Immunology in
comparison with other relevant studies.
a- The Ogasawara study1
In their study, Ogasawara and collaborators included a large set of patients
with RPL (n=1309) who had between 2 and 20 consecutive first trimester
losses before a subsequent pregnancy1.
They did not select for euploid losses as we did here at BRI and still
had exclusions in their study where we had none.
Immune therapy was administrated to patients with at least 3 prior pregnancy losses.
In their study, 65% of RPL patients (2 or more losses) managed to have a successful pregnancy, with treatment
compared to 77.8% for our patients here at Braverman Reproductive Immunology. When considering patients with at least 5 losses, they have a
35% success compared to 80% for us at
BRI. The pregnancy success rate should have been higher and the number of
euploid losses (49%) should have been lower if the therapy was appropriate.
b- The Morikawa study2
In this study, the authors studied 75 cases of RPL patients with at least
2 prior losses. They found that
38% would have a successful pregnancy compared to
78% for our treated patients here at Braverman Reproductive Immunology. And
most of the losses in their study (67%) are euploid showing again that
the therapies that they provided were inadequate and/or inefficient to
sustain a euploid pregnancy
c- Where do we stand in comparison with other reports?
We had a higher overall pregnancy success rate in patient with one or more
euploid losses compared to both Ogasawara (p=.01) and Morikawa studies
(p=.0001). At
first attempt to conceive, we had71% of pregnancy success as shown in Figure 5 and we have to highlight that our overall pregnancy
success rate of 77.8% is reached with a
maximum of three attempts.
In patients with < 5 losses,our pregnancy success rate reaches the outstanding value of 80%, that is much higher than Ogasawara study (p=.0001, low p value shows
a high statistical significance).
This shows that our immune therapies are highly adapted and effective in
retaining euploid pregnancies.
References
- Ogasawara M, Aoki K, Okada S, Suzumori K. Embryonic karyotype of abortuses
in relation to the number of previous miscarriages. Fertil Steril. 2000
Feb; 73(2):300-4. PubMed PMID: 10685533.
- Morikawa M, Yamada H, Kato EH, Shimada S, Yamada T, Minakami H. Embryo
loss pattern is predominant in miscarriages with normal chromosome karyotype
among women with repeated miscarriage. Hum Reprod. 2004 Nov; 19(11):2644-7.
- Carp H, Toder V, Aviram A, Daniely M, Mashiach S, Barkai G. Karyotype of
theabortus in recurrent miscarriage. Fertil Steril. 2001 Apr; 75(4):678-82.